I recently attended a meeting of the Patient and Public Interest Group (PAPIG), which is made up of patients, carers, patient advocates and third sector organisations. The group feeds their views via the All Wales Therapeutics and Toxicology Group (AWTTC), who provide professional, technical and administrative support to the All Wales Medicines Strategy Group (AWMSG). One of the roles of AWMSG is to advise Welsh Government whether new medicines should be available for use in NHS Wales.
New medicines are evaluated against currently available medicines to compare:
- how well they work,
- how cost-effective they are,
- which patients they would benefit the most.
AWMSG is committed to involving patients, carers and members of the public when evaluating new medicines. During the appraisal process, the patient and carer view is critical because clinical data alone can’t quantify a patient experience – the patient needn’t be an expert in medicine in order to be involved in this process. Most of the questions asked of them during the appraisal process are related to their condition and how it affects their day to day life.
The patients and carers who contribute may not be scientifically or clinically trained, but they certainly hold invaluable knowledge about the impact that their condition has on their and their families’ lives. Other stakeholders such as pharmacists, academics, clinicians and industry representatives are also involved throughout the process. The patients and members of the public are found through patient advocates and third sector organisations that are represented on Patient and Public Interest Group. AWTTC also search for other patient groups in order to reach those who are not currently engaged in this process.
It’s worth noting that other bodies in the UK who appraise new medicines do not take responses from individual patients or members of the public, but AWMSG do.
Patients and members of the public who are involved are known as lay-members. The dictionary definition of a lay-member is “A person who does not have specialised or professional knowledge of a subject.” So if this is what a lay-member doesn’t have, what about the skills that they do have?
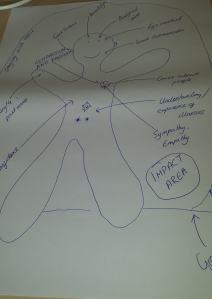
At the meeting, we completed a participatory exercise to examine ‘what skills, experience, qualities and attributes does a lay member have?’
Here’s some of what we came up with:
- Getting the point across
- Analytical ability
- Good communicator
- Good understanding and experience of health conditions
- Good listener
Qualities and attributes
- Confident
- Sympathetic / empathetic
- Caring
- Being able to stay within their remit
Completing this visual exercise was very a thought-provoking and interesting way of looking at the lay-member role.
What participatory tools have you used to analyse the roles of citizens involved in your consultation process?